Hospital After Home
HOSPITAL BIRTH AFTER TWO HOME BIRTHS
The Birth of Kevin Robert Wiener, October 19, 1985
by Rosemary Romberg (Wiener)
I am fortunate to be the mother of five* healthy children. Each baby’s birth has been unique. Each were positive experiences, with natural births by the Lamaze method. Each one was in a different place, with a different birth attendant, and except for my husband, with different people assisting me.
Our first son was born in 1972. At that time natural childbirth and husband participation were extremely new, innovative concepts. We thought we were being quite progressive at the time. The hospital staff passively cooperated by not offering me medication during labor or birth and by allowing Steve in the delivery room. But after Eric was born the three of us had to go our separate ways. The baby was whisked off to the central nursery. I was put in a recovery room. Steve was sent home. Eric was brought to me for the first time the following morning 12 hours after his birth. I did not get to know my baby until we went home two days later. Later we came to realize how much we had missed out on because of this senseless, but routine, separation after our baby’s birth. People today are horrified at such practices, but at the time this was the norm. New parents today often fail to realize how hard leaders in the field of childbirth education have had to work to change such practices within hospitals.
I became a childbirth instructor a few months after our first child’s birth and soon learned a great deal more about birth and babies. Our second son, Jason, was born 2 ½ years later in 1974. His birth was in another hospital which was extremely progressive and innovative for its time. It was so special to be able to hold the baby immediately after birth on the delivery table (although he was wrapped in blankets) and then have uninterrupted rooming in shortly thereafter. This time Steve and I did not have to be separated from our baby. But I did miss little 2 year old Eric terribly until I went home two days later. At that time including children in birth, or even letting them visit in the hospital after birth was totally unheard of.
Two and a half years later, in 1977, our third son, Ryan was born at home. Leboyer’s book Birth Without Violence was becoming popular, although most hospitals were still reluctant to take up such a radical practice. Our extremely progressive doctor who supported immediate bonding had left the area. Few other doctors were “liberal” enough to “allow” immediate mother-infant contact. We wanted total control over our birth. We did not want to have to cater to hospital rules or doctors’ whims. At that time home birth was a radical departure from the traditional way of handling birth in virtually all hospitals. Home birth was the only way I could have stayed in the same bed to have my baby (rather than be taken to a delivery room.) It was the only way I could have had immediate contact with my baby (not to mention skin to skin contact). Also a midwife’s gentle, informal, feminine approach to birth was so much less threatening than the more detachedly “professional” approach of even the nicest of doctors. (Midwives rarely practiced in hospitals at that time.) Our two older children, then ages 5 and 2 ½, were present for Ryan’s birth and this was one of the most beautiful features of all. Ryan expressed an almost ethereal peacefulness which I had never seen before in my other babies. I felt an immediate sense of love and bonding for my baby that had taken much longer to develop with my first two babies.
To have Ryan at home we had to go underground. You had to know the “right” people and be somewhat trusted to even find a lay midwife. (This is because the authorities were out to arrest midwives!) Licensed, “established” midwives were virtually non-existent then. Alternative birth centers were not available either. Only a few existed in the entire country, and none in our local area.
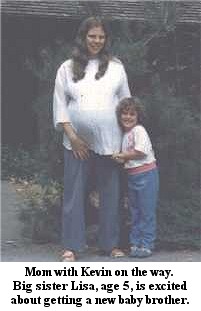
Four years later our fourth child was on the way. By this time we had moved from southern California to Washington state. Birthing practices had become somewhat more progressive and home birth was less “underground.” I readily contacted a local lay midwife and again made plans to give birth at home. While the idea of home birth while carrying Ryan in 1977 had seemed extremely radical and daring, this time it was just the way it was going to be. In January of 1981 our daughter Lisa was born at home, again with absolutely no problems.
I considered myself an extremely healthy, low risk mother who had my babies naturally and easily. I would never have imagined that I of all people, would soon turn into a “high risk” mother who would experience devastating loss twice in a row and would end up again embracing hospital services, however reluctantly. Home birth was just the way I had my babies by now. I could not have imagined ever even considering hospital birth unless I were faced with certain, dire, grave, complications.
The story actually begins when I was in early pregnancy with Lisa in 1980. At my 11th week I saw a doctor (for back up care) who said that my uterus felt as large as a 15-16 week pregnancy. We discussed the possibility of twins or being further along than I thought, but he said it was probably fibroid tumors that caused my uterus to seem somewhat large and irregularly shaped. I scarcely knew what fibroid tumors were. He gave it no further concern and neither did I. I carried Lisa to term and gave birth to her at home with no problems. Little did I know that one day fibroid tumors would be the nemesis of my life.
In 1983, shortly after Lisa turned 2, I found that I was pregnant again. I was 36 years old at the time and the baby was due in November of that year. My midwife who had attended Lisa’s birth had gone into nurse’s training and was no longer midwifing. So I contacted another well known midwife, “W”, whom I already knew to be an extremely likeable person. There was absolutely no question in my mind that I would have another home birth.
At my eighth week I had my first visit with her. She told me that my uterus seemed like a 12 week pregnancy, she readily detected a fibroid tumor that was about the size of a hen’s egg along one side. This seemed like a repeat of what the doctor had told me 2 ½ years earlier when I was in early pregnancy with Lisa, so I gave it little concern. But she was worried about the prospect of the fibroids causing postpartum hemorrhage and had me contact the same doctor I had seen before. A decision about home birth was tentative, resting on the prospect of an ultrasound during my eighth month to locate the exact position of the fibroids. They were also talking about her giving me IV fluids at home. I was still very much anti-technology and wasn’t sure whether or not to agree to any of this! I was somewhat defiant about their overly worried “medical” attitude, and was considering doing it myself, or finding another midwife, just to get away from their hyper-conservative approach. After all I had already had four babies easily, two at home, and I had had fibroids before during my pregnancy with Lisa and it hadn’t been a problem then.
All that flippancy and defiance on my part changed fast in June of 1983 when much to my severe shock I lost that baby at the 19th week of pregnancy. With the death of that baby began the death of that old, self-sufficient, semi-rebellious self — a long, slow, painful “death” and joyous “rebirth.” That miscarriage was followed by severe grief, and over a year’s worth of Herculean but futile attempts at healing myself. These included “wholistic” health remedies, dietary changes, “positive visualizations”, etc., in the hopes of eliminating that tumor from my body, so that I could carry another pregnancy to term and have another baby. I would not be “healed” from that catastrophe until that could be accomplished. I considered myself an extremely strong-willed, self-sufficient person, able to get whatever I set out for.
An ultrasound five weeks after the miscarriage confirmed the presence of a fibroid tumor cluster about 5-6 cm. in diameter in the upper right area of my uterus. But manual examination 10 months later by the same doctor indicated that it had apparently regressed, and was no longer palpable. The tumor had apparently caused the miscarriage by blocking nutrients from reaching the placenta so the baby could not continue growing. This was an extremely horrifying thing for me to deal with — that there could be an alien being inside my uterus that killed my baby!! But now, the following year, after months of determined juice fasting, total vegetarian diet, extensive “positive visualization” (among other things) gave me nearly normal prospects of carrying a future pregnancy to term. I became pregnant again in May of l984. That baby was due in January of 1985. Again “W” accepted me for a home birth, this time unconcerned about the fibroids since my uterus seemed normal sized this time and no tumor was palpable upon examination.
To make a long story short, I lost that baby also, in September of 1984, again at 19 weeks, in a manner almost identical to the one before. (The details of both of those miscarriages are shared in my new information sheet entitled Coping With Perinatal Loss which is also available on this website.) Click here for article
Following that miscarriage I gave up on the idea of ever having another baby and decided to seek spiritual healing alone. To make yet another long story short, I have found healing through Jesus Christ. I have experienced the apparent complete disappearance of the tumor along with the successful pregnancy and birth of our full term, healthy son, Kevin, who was born in October of 1985. I am actually an unlikely person to find myself turning myself over to Jesus for healing, and then to my great astonishment finding this real after all other attempts at healing had been futile. Prior to this experience I was much too “sophisticated” and “liberal” in my thinking to ever consider traditional Christianity as any path I would ever want to follow. So the story of my finding Him in my life is both incredible and unconventional.
 I did not have the courage to even think about attempting another pregnancy after losing two in a row, even though I was filled with an intense, irrational “baby-hunger.” But I prayed about it and Kevin was an answer to many prayers. In January of 1985, about four months after the last miscarriage I became pregnant again, despite precautions. I was undergoing an intense amount of personal, spiritual healing, along with closeness to the Lord, and two days after my period would have been due I woke up and realized that I was pregnant and I knew in my heart that everything would be okay this time. I felt a strong sense of faith which carried me through the next four weeks or so. Then when I was about 8 weeks along my new found faith began to falter and I vacillated between total trust and faith in the Lord that this new pregnancy would make it to term, and absolute, devastating, crushing fear that I would have yet another miscarriage and the nightmare of the past two years would still be continuing.
I did not have the courage to even think about attempting another pregnancy after losing two in a row, even though I was filled with an intense, irrational “baby-hunger.” But I prayed about it and Kevin was an answer to many prayers. In January of 1985, about four months after the last miscarriage I became pregnant again, despite precautions. I was undergoing an intense amount of personal, spiritual healing, along with closeness to the Lord, and two days after my period would have been due I woke up and realized that I was pregnant and I knew in my heart that everything would be okay this time. I felt a strong sense of faith which carried me through the next four weeks or so. Then when I was about 8 weeks along my new found faith began to falter and I vacillated between total trust and faith in the Lord that this new pregnancy would make it to term, and absolute, devastating, crushing fear that I would have yet another miscarriage and the nightmare of the past two years would still be continuing.
I still wanted very much to have another home birth. I called my midwife “W” when I was only seven weeks along. But she insisted that I should go to the doctor this time. I then made an appointment with him. It was impossible for me to think ahead to the birth. Most people facing normal pregnancies can afford that luxury, but a woman who has miscarried twice in a row does not dare look ahead to the prospects of giving birth to a healthy, full term baby!
The doctor was sympathetic and supportive, but of course there was nothing in his power that could make the pregnancy go to term. It was all just “wait and see.” He did not have me come in for any more appointments than normal for a woman in early pregnancy.
For the first 18-20 weeks I told very few people that I was pregnant, and refused to make any plans for the baby. I had sold or given away practically all of my baby things shortly after my last miscarriage, but I refused to get any new maternity clothes or baby things until I passed the point that I had lost the others.
By the time I reached my 16th week I became more apprehensive. This would be “do or die!” My last pregnancy was so recent that I could still distinctly remember what it had felt like at that stage, especially the failure of my uterus to get any bigger, the loss of nipple sensitivity and normal pregnancy feelings, and the horrible deadness and wrongness inside. By my 17th week I realized that my uterus was definitely bigger than it had been the week before, and that I still felt “pregnant.” There was a total sense of “rightness” and “healthiness” about this pregnancy that I so clearly remembered was lacking during the last two just before I had miscarried. At my 18th week I saw the doctor again and much to my immense joy the baby’s heartbeat was loud and clear when he checked it with the Doppler. After the appointment was over I sat in my car and cried and cried with relief and thankfulness that my prayers were finally being answered.
I called my midwife “W” again with the joyful news. Everything was fine!! I was a healthy, normal mother having a baby again’! This baby was going to make it!! But while she was happy about the news, she did not share my optimism. “No, Rosemary, I just feel really strongly that I shouldn’t be your midwife. Not after you’ve lost two babies in a row. You’re just not a midwife’s patient.” I was disappointed and especially let down by her. I had become quite close to “W.” over the last two years, sharing my grief over my losses. Couldn’t she share in my joy and healing now?! No, the “statistics” were against me. I was 38 years old. It was my 8th pregnancy. (I also had one other early miscarriage back in 1973.) This would be my fifth (full term) baby. I had fibroid tumors and I had lost two babies in a row. She couldn’t see beyond that. But I had already had four perfectly normal, easy births. I had had two home births already. I’m just not a hospital person. Can’t she see that I’ve healed? “If you really want to have a home birth, I’m not saying you shouldn’t have one. But I just shouldn’t be your midwife this time.”
I wasn’t sure what to do. I had saved an article in our local paper about another midwife, “R”, who did deliveries at a well known birth center in a nearby community, Mt. Vernon. She was soon to be doing deliveries in our local hospital as well. Maybe this was the answer! She sounded quite nice, personable, and spiritual. I liked my doctor very much, but by now I was so accustomed to a midwife’s more feminine, personal style of care. A midwife’s way is usually so much more patient, non-threatening, and non-interventionist. If I have to have the baby in a hospital, at least if I could have a midwife, maybe this would help me bridge the gap. I made an appointment with her when I was 21 weeks along. I also toured the local hospital to ask questions about their maternity department. It was the same hospital where I had been cared for during my last two miscarriages, but this time, of course, I saw it from a completely different perspective. They were planning all sorts of changes in the near future but not soon enough for my upcoming birth. I told them about my previous miscarriages and my previous home births and how hard it was for me to face a future hospital birth
They had one small birthing room. It looked drab, like a storage room with one small, narrow bed in the middle. Most of their births were traditional labor room/delivery room births. Not too many people requested the birthing room, but they were understanding of my needs. Of course I also couldn’t be guaranteed that no one else would be using it. Next year when their new birthing suite would be finished they would have several attractive, up to date birthing rooms. They did allow siblings, friends, spouses and any other support people in for the birth – as many as desired. Things had come a long way. I felt neither horrible, nor terribly excited about giving birth there. My new midwife had not done any births there yet. Things may change even more once she gets accustomed to practicing there.
I then had my first visit with the midwife, “R.” She was a sweet, friendly lady in her 50’s and seemed very much understanding of my position. My first appointment took place in the birth center where she also practiced. She said something about the possibility of my giving birth in the birth center there if I preferred. Then she said, “No, with the prospect of fibroid tumors, I don’t think you’re a candidate for the birth center. We’d better stick with the hospital.” I felt quite comfortable about being under a midwife’s care, and was just beginning to accept the reality of this pregnancy going to tern.
First she wanted an ultrasound. I was a little reluctant. The only other time I had had one done was after my miscarriage in 1983, and I had not been pregnant then. Could this possible damage the baby? My old, back to nature, anti-technology self would have spurned something like ultrasound. But the part of myself that had lost two babies desperately needed the reassurance that this baby and pregnancy were okay. The ultrasound was fascinating. It revealed a placenta that was to my back, and a “myomatous thickening” towards the top of my uterus. (“Myoma” is the medical term for tumor.) It wasn’t the definite tumor that had been apparent two years previously, but just a thickened area that seemed to begin where the placenta ended. (Part of the miracle that I experienced is that normally fibroid tumors tend to grow with the pregnancy because they are stimulated by the hormones of pregnancy.) Nothing was threatening this baby’s placenta. The ultrasound also revealed a perfectly normal baby (as far as could be determined.) I asked to know the sex and the technician told me it was a boy. I was glad to know, but it was a weird feeling knowing that in advance.
Interestingly, by dates I was due on October 9th, but according to the ultrasound’s assessment of the baby’s development, I wasn’t due until the 26th, so I was never sure. I never had any ultrasounds done during any of my previous pregnancies. I wonder if they would have had similarly discrepant due dates had it been done with any of my others.
The summer continued with my pregnancy blossoming normally and the baby kicking and growing every day. My due date and the prospects of birth still seemed ages away, but suddenly it was all catching up with me. I liked my midwife, but I wasn’t happy about the prospects of having a hospital birth. She still had not delivered anyone at our local hospital and it looked like I would be her first client there. I did not like the idea of being a ground breaker for such a prospect. She and I might be fighting the system for all sorts of things. I did not want to have to be doing that. I just wanted another peaceful, untraumatized birth.
I then wrote a long, pleading letter to my ex-midwife, “W”. Logically it did not seem to me that this pregnancy was in any greater danger than my last two pregnancies would have been had they been implanted differently and gone to term. She had accepted me for a home birth with both of them. It did not seem that any greater potential danger with this pregnancy was at issue. It seemed that I was just being penalized because I had lost the last two babies. I urged “W”, “Let’s just forget all this hospital nonsense and have a home birth like I’m supposed to. With a home birth I would feel completely healed. But running to the hospital meant that we were still clinging to all the grief, pain and complications of the past two years.
She understood my feelings, but still refused to take me. At the outset of my pregnancy when I had first approached her she had written a letter to my doctor (who was her back up doctor) informing him that she would not be taking me as a home birth patient for this pregnancy. Therefore, she felt that if she changed her mind and took me now, and then I did have complications and she had to call on him, she would be in trouble and he would refuse to cooperate. It was all politics. Couldn’t I take responsibility for that?!! I was caught up in the middle of their politics and fears. She urged me to contact another home birth midwife, “S”, whom I already knew and liked. She had been an assistant to “W” in the past and I had seen her at some of my previous prenatal appointments when pregnant with my miscarried babies.
Meanwhile my due date was growing closer and closer, and I still wasn’t certain or at peace with any available option for giving birth. I can understand midwives’ fears, but to be caught up in the middle of them and be ostracized the way I was is extremely painful as well. “Criteria” for home birth mothers makes a lot of sense on paper, but can be terribly painful and unfair when you are the one being discriminated against, especially when it seems to be with no respect for who you are in relation to your needs, feelings, and lifestyle. I felt reduced to a bunch of statistics. To get this kind of treatment from someone I had felt especially close to was especially frustrating and unnerving.
I then shared my feelings about this with “R” and told her that I had spoken with “W” again about home birth. “R” still felt that I should give birth in the hospital, but finally conceded that “if I felt that strongly opposed to having a hospital birth, she would deliver me in her birth center.” She could get me to a hospital from there in ten minutes if necessary, but did not believe that I could be transported that quickly from home. (I live about 15 minutes from our local hospital.) Then we found out that our insurance would only pay for hospital services. It would cover the midwife’s fees regardless of location, but did not recognize the free standing birth center as a legitimate place to give birth. That would have cost us an extra $500 for a setting that would not be that much different from the hospital. Forget it!
She then urged me to tour the hospital in Mt. Vernon where she had been doing deliveries for some time. They had just remodeled their maternity department and were having a special open house. I was considerably more impressed with this hospital than I had been with the local hospital in Bellingham. They had three new birthing rooms that looked just like bedrooms with attractive wallpaper, bedspreads, and special birthing beds. Their emergency supplies of oxygen and medications were conveniently concealed inside the walls. It looked quite comfortable and inviting. Only the electronic fetal heart monitors sitting on the tables beside each bed set me aback. No way was I going to give birth wired up to machines and monitors!! I’d be sure to talk to ”R” about that later. I asked the nurse who was giving me the tour a lot of questions. They sounded quite flexible about many of the things that concerned me such as waiving the vitamin K shot and ointment in the baby’s eyes, and being able to keep the baby with me from birth on. They had a requirement that one had to stay there for a minimum of four hours after giving birth. Of course I’d go home just as soon as I could and that sounded fine. It didn’t look so bad. My friends, husband and other children would all be there for the birth. If I could manage to eliminate many of the routine hospital procedures that I was so against, maybe giving birth here would be okay.
I was still in a quandary about it, though. Some days I was feeling completely content about going to the hospital. Other days I just had to find a home birth situation I could feel comfortable with! This just couldn’t be me, planning a hospital birth after being a committed home birth mother for so many years!! Many nights I lay awake tossing and turning about my decision.
I finally called “W’s” former assistant “S” about it and she and I had a nice talk. Maybe she would attend me for a home birth. Maybe this would be the answer. Like everyone else, she was concerned about fibroids and the threat of hemorrhage. By this time I was nearly 36 weeks along and was scheduled to have another ultrasound. “S” and I decided to delay any decision about home birth or whether or not she would take me until I had the report from the ultrasound, in regards to the size and location of the fibroids. The ultrasound revealed wonderful, miraculous news! No abnormal uterine tissue!! I know that I’ve healed, and I know Who’s healed me! Joyfully I relayed the news to both “W” and “S”, but they still refused to believe me. “The baby was probably concealing it.” They just couldn’t believe that it could be gone. “W” still felt bound by her promise to the doctor that she would not take me, but “S” would not be bound by any such agreement. Still, she was equally unyielding. No way was she going to take me, even with a provenly fibroid free uterus! In absolute frustration I screamed at her over the phone. “There is nothing wrong with me!!! I don’t have fibroid tumors!! I’ve had two home births already!!” But she refused to be persuaded.
There was a time when I would have almost certainly given birth at home by myself had I found myself unable to find assistance for home birth. But that was before I went through the trauma of losing two babies in a row. I know that I was not totally dependent on those two ultraconservative midwives. Still, I had a greater need for security and assistance with birth than I ever had before. In retrospect I wish I could have done it differently. I wish I had had the courage to give birth on my own, but at the time the grief over my lost babies was too fresh and I could never have gotten my head together enough to do it that way. I needed support from a qualified source and since I couldn’t get it the way I wanted to, i.e. for a home birth, I’d have to make a lot of compromises.
I also considered contacting one or two other unofficial “lay” midwives in town that I knew of. But I didn’t know them very well. By this time my due date was getting closer and closer. My midwife for Ryan’s birth 8 and ½ years before had been a lay midwife, just beginning her practice, so it wasn’t the lack of “official” qualifications that concerned me. Had I started out much earlier with one of them I’m sure I would have felt perfectly okay about it. But by this time it was just too late to make changes. I had a good rapport with “R.”. Besides the hospital in Mt. Vernon did seem quite nice and inviting, if I could just manage to make my needs and wants clearly known.
I wrote up a detailed list of my birthing requests and gave a copy of it to my midwife. Another copy went in my suitcase to have ready while in the hospital. Many of my requests were easily accepted without any problems: Older children, husband and friends present, baby not to go to the nursery as long as all is normal, use of our own nightgowns, etc., for myself and for the baby, no supplementary bottles, etc. For other options I’d have to sign waivers, pull a few strings, and be assertive. If I wanted no ointment in the baby’s eyes, as I was insisting, I’d have to have a gonorrhea test done shortly before my due date. These types of things are taken for granted at home, but when dealing with a hospital you have to know what you want and don’t want, and sometimes go to extra trouble to see that they are realized.
Most importantly, however, I made sure my midwife knew that I did not want to give birth wired up to machines and monitors and all that junk!! She can check the baby’s heartbeat from time to time with the fetascope or hand Doppler if she wishes, but unless something was terrible wrong, no way was I going to be wired into that monitor! That’s just not the way I give birth. Ditto for the I.V. I had had a routine I.V. back in 1972 when Eric was born, but that was in the “dark ages.” I had Jason, Ryan, and Lisa all without I.V.s stuck into my arm, and I didn’t need to give birth feeling like a pin cushion!! I didn’t even want the “heparin lock” that “R” had mentioned, which is a small plastic needle stuck into a vein just to keep it open in case of hemorrhage, shock, and sudden emergency need for an I.V. If I have to go someplace else to give birth to make everyone else happy, then that’s the way it has to be. But I still wanted to give birth naturally, without feeling like a computer or a voodoo doll!
By this time I had also had several visits with another midwife, “M”, who alternated practice with “R” She was much younger than “R”, in her 30’s like I was, and she and I hit it off very nicely. Sometimes she took “R’s” patients if “R” was busy or tired. Much as I liked “R”, I found myself hoping that “M” would be on call when I went into labor. She seemed more understanding of where I was coming from, my wants and needs for birth, my yearning to be free of hospital technology, and my feelings of loss over not having another home birth.
By now the final days of pregnancy were upon me, and I felt huge and ominous. The 9th of October came and went. The most recent ultrasound had given me a due date range of Oct. 22nd through Nov. 18th. I could hardly believe I would go that long. On the 15th I had the obligatory gonorrhea test, amidst a certain amount of consternation from the laboratory personnel. “They use erythromycin drops now instead of silver nitrate, which aren’t so stinging or painful,” they assured me. I’m sure they didn’t understand what I was so concerned about. For me it was largely “principle.” I knew we didn’t have gonorrhea. At home it had never been a question. But I was going through these “hoops” for them.
Each day I felt heavier and more ready. Braxton-Hicks contractions continued with constant regularity. Occasionally I’d wonder if I was going into labor and feelings of dread and panic would overtake me. Usually I pushed the reality of labor and birth out of my mind, but I knew I’d have to face it soon. Despite my new found spiritual healing, I was still facing labor and birth with feelings of fear and dread that I had never known before. The pain and losses over the last two years had taken a heavy toll. Ever since I had lain there in bed for six hours back in June of 1983, waiting to pass that little, limp, dead fetus, I have never been the same person. Even though this baby kicked and moved constantly with life force, I had an abnormal dread of the baby being born dead! That possibility had rarely entered my mind back when my other children had been born.
On I Thursday, the 17th, I was examined again by “R” who said I was dilated to 2 cm. already, although not effaced. She and I both knew it wouldn’t be much longer. I could hardly believe that after all this time there would actually be a baby here soon. On the morning of Friday, the 18th, I went to the bathroom at about 9 a.m. and had kind of a “natural enema.” After that I felt extremely achy in my pelvic region. I was concerned that something might be happening, but I took a nap for about an hour and the aching went away.
Besides writing, I also sew a lot. My old sewing machine had broken down two weeks before and we had been looking at new ones. That night we purchased a new electronic machine that does all sorts of fancy stitches and extra things. I was excited about having a new “toy” to play with.
I woke up on the morning of the 19th at about 6 a.m. As I lay there in bed I felt a couple of Braxton-Hicks contractions that were quite achy and about 15 minutes apart. But then I got up, went about my business and forgot about the contractions. I spent much of the day trying out my new sewing machine, including decorating some pillow cases and some new white flannel diapers. I didn’t feel like eating much that day. By early afternoon I realized that contractions were hitting regularly, about fifteen minutes apart. I did slow deep breathing with each one, and they were mildly achy. I was able to operate the sewing machine all this time and concentrating on it made a great focal point. I still wasn’t sure if this was real labor, although as time went by I became more and more suspicious. I was conditioned to expect my water to break. Jason’s, Ryan’s, and Lisa’s births had all begun with my membranes rupturing, as had my two recent miscarriages. Whenever that happens there is absolutely no question that ”this is it!!” Only Eric’s birth long ago had begun with contractions like this. When that happens it takes a while before you are sure if this really is labor. This continued throughout the afternoon, but I still hadn’t told Steve or anyone else how I was feeling. Steve took off with Ryan and Jason to get them new shoes. I was relieved when they got back. Finally it was around 6 p.m. when I looked at my bulging belly and said to the baby inside, “I think you want to come out now, don’t you?!” It was time to get dinner, but I told Steve I was going to call my midwife. He got dinner together for himself and the kids. I didn’t want any and I nibbled a few pieces of dried fruit instead. “M” lived in Bellingham, so I decided to call her first to see if she could just come over to check me. But she wasn’t home. Then I called “R”, and she and I decided together that I would go to the hospital just to be checked. With each contraction I was becoming more sure that I really was in labor! I laid down on the bed and had a couple more contractions before calling my friends, Sherry and Susan. Sherry wasn’t home. Susan was very excited about my birth and said she’d meet us there at the hospital. I took a shower and put on a new nightgown and my bathrobe. By 7 p.m. we were putting suitcase, kids, sleeping bags, etc. into our van and were on our way. I filled a large plastic cup with orange juice to sip along the way as I knew that this would help keep up my energy level.
The drive to the hospital was about 45 minutes from our home. The contractions were about 5 minutes apart by now and were no longer as mild as they had been all day. I was having to use regular “hee-blow” breathing for each contraction. It was dark outside and there wasn’t much that I could use for a focal point. I was sitting up in the front seat and during every contraction I felt every little bump and turn the car made. Chalk up one point here in favor of home birth. Experiencing strong labor contractions while riding in a moving vehicle is not at all comfortable!! I would have been much happier staying home and letting every one come to me.
Soon we were at the hospital and I was whisked upstairs to the birthing suite. Susan was already there waiting for us. The kids were quickly settled into a waiting room complete with their sleeping bags, books and crayons. There was a refrigerator in there full of juice, popsicles and assorted goodies which the kids dove into!
“R” had arrived. She checked me and found I was dilated to 3 cm. and 90% effaced. I was obviously in labor. I settled down onto the bed. I handed her my “birthing plan” full of “wants” and “don’t wants.” I didn’t have an enema or a pubic shave – I don’t think they did them there routinely anyway. The nurse proceeded to check the baby’s heart tones. She held the heart monitor to my abdomen by hand and listened to the heartbeat through one contraction. They sounded loud and clear. Normally the heartbeat slows a little during the contraction and picks up when it is over. The nurse was concerned that it was not recovering as quickly as it should after the contraction held ended. “We’ll have to check it through a few more contractions to be sure,” she told me. I then heard her say to another nurse. “This way we’ll have a record if anything does go wrong.” I’m sure that is what they are taught.
I was moved to a larger birthing room since I had so many people in tow. I had brought along some herbal tea especially intended for use during pregnancy. Susan made up some for me with honey in it. I drank a couple of cups. This was on top of the orange juice I had sipped on the way. Soon I had to go to the bathroom. They asked me to give a urine sample. After checking it they promptly informed me that my “ketones” were “dangerously high”, indicating that I was dehydrated and would have to have an I.V. “You would have to drink at least 16 cups of that tea to bring it down to normal,” “R” advised me.
No one had ever checked my urine during labor when any of my other babies were being born. I wonder what my ketones were like with each of them. I gave birth to my last three babies just fine without any I.V. But “R” was quite insistent on talking me into it.
“Will I still be able to use the bathroom if I have it?” I asked. I remembered being forbidden to get up, even to use the toilet once the I.V. was in place, when I had been in labor with Eric 13 ½ years earlier. “R” assured me, yes, of course I could still use the bathroom, so I resignedly agreed to it. I was feeling somewhat fatigued already and knew that labor would get much harder before I was through. Also I had become well acquainted with I.V.s during my last two miscarriages.
Everybody got into watching my contractions and the baby’s heartbeat on the monitor. I actually found it quite fascinating, – not as alien or disturbing as I had imagined. To the anti-intervention, “back to nature” part of myself, again, dependence on such a device seems like anathema. But to the self that lost two babies over the past two years, every beat on that monitor means “my baby is alive!!” This is an abnormal state of mind, to be sure, but understandable in my position. And of course hospital personnel see their portion of tragedies which similarly distorts their perception of normal birth. The medical profession is usually overly cautious, conservative and/or interventive about such matters. On the other hand, some home birth advocates are appallingly flippant about pregnancy complications and birth tragedies. Some seem to insist that birth complications and tragedies either “don’t happen” or “don’t matter” and both of those assumptions are blatantly false!
Heart monitors are sometimes criticized as robbing the mother of the human contact and attention that she needs during labor. But at least in my case this was not true. My midwife, two nurses, two friends and my husband were with me constantly, while my oldest son popped in and out of the room from time to time. I received constant attention and was anything but neglected and left alone! (I was the only patient in labor there at the time, which probably was partly why I got so much undivided attention. Also, because I was a fifth time mother they undoubtedly expected my labor to proceed rapidly.)
I learned a great deal about heart monitors from this experience, much of it extremely interesting. The baby’s heartbeat jumped around a lot, sometimes registering in the 120’s and sometimes as high as the 170’s. My midwife said it was probably doing that because of my ketones being high. (I still do not understand how that affected the baby, but then I’m no chemist!) We also found that the heart tones were more depressed when I lay on my right side than on my left side, so I stayed on my left most of the time. (I have always wanted to stay lying down on one side during all of my labors, so I did not feel hampered by this. I suppose someone who would rather be up walking and moving around would find the device more restricting.)
“R” also mentioned the possibility of using the internal heart monitor should the need arise. (This is the electrode device which attaches directly to the baby’s head before birth to give a more direct reading of the heart beat. So far I had only had the external monitor.) I was sure that my baby would never be in any kind of trouble that an internal monitor would be called for! The conversation was merely an academic one to me. “Oh, I’d sure never want that used unless there were dire complications. When I used to teach Lamaze classes, I had a student whose baby developed a scalp abscess where the monitor had been inserted. The baby lived, but she had been sick for several weeks and had been given a 50-50 chance of surviving!” I told her. I’m sure “R” knew I was not at all keen on the internal monitor.
“Oh, it’s such a tiny little filament that is used now,” she assured me. “Almost always you can’t even see the place on the baby’s scalp where the monitor was inserted.” The baby’s heart beat continued strong and healthy on the monitor. My baby’s head won’t be traumatized by any electrode stuck into him!! That was just out of the question as far as I was concerned!!
Soon I needed to go to the bathroom again. I started unfastening the monitor belts, but the nurse told me to just leave them on. That trip to the toilet was a bit ridiculous. Susan hauled the I.V. stand along beside me. The monitor belts were flapping and clunking around all over the place. I managed to use the toilet amidst all that paraphernalia, and then quickly get back into the birthing bed, having a couple of contractions along the way.
At around 9 p.m. “R” examined me again and found I was dilated to 5 cm. and totally effaced. My membranes were soft and bulging. We discussed breaking them. She assured me that doing so should speed up the progress of my labor. I was all for it. She broke them and a surprisingly small amount of fluid came out.
Labor continued with each contraction getting a little stronger and sharper than the last. I used the monitor for a focal point much of the time.
In the meantime we had managed to call my other friend, Sherry and she had come to the hospital as well. Now she was helping too. My lower pelvic bones were aching constantly, so Sherry and Susan soaked towels in hot water and put the hot compresses on my hips. This greatly helped ease the ache. I have always found the last hour or so of labor (transition) extremely difficult and painful despite all the Lamaze and other relaxation techniques I can muster. This labor was no exception, Everyone was telling me how well I was doing and how relaxed I seemed. (I guess all maternity departments see their share of real screamers and panic stricken women!) I felt like I was barely hanging on!
At around 11:30 the pushing urge started to come with the contractions. It was almost impossible not to push!! Things were happening extremely fast now!! The kids all came in to the room to watch. Suddenly the baby’s heart tones could no longer be picked up on the monitor! Everything was in a blur! I heard “R” ask me, “Rosemary, is it okay if I check the baby’s heartbeat with the internal monitor?” She had the electrode in her hand, ready to insert. I was scarcely familiar with the workings of the monitor, and late transition is hardly the time for rational thought. Yet I could easily figure out that the baby was just moving down into my birth canal and away from where the monitor picked up the heart beat from the outside. I didn’t think that there was anything wrong with the baby. Between contractions I tried to answer, “Isn’t the baby coming down now?” I didn’t want that electrode in my baby’s head. Still I wasn’t able to be assertive enough to insist, “NO!!” I was afraid of jeopardizing my baby either way, and things were just happening too fast!
A nurse slapped an oxygen mask over my mouth and nose. I wanted to yank it off! It was an uncomfortable feeling. But then I saw a number on the monitor! My baby’s still alive!! I had to let it stay on and breathe that pure oxygen so I can make sure my baby’s okay!
The next contraction was horrendous. Suddenly the baby’s head was crowning, pushing, burning, stretching, … stretching … stretching, … instant relief. I had refused to hold back and allow my perineum to gently stretch and ease the baby out. I had hurried because I had to get him out but I didn’t want any electrode in his head either!! I managed to save him from both dangers!! I recall all of my other babies being born fairly slowly, the head emerging first and then a pause before the body slowly came out. But this time the baby fairly flew out in a sudden plop!!
I sat up and stared at the tiny boy lying on his back in a puddle of blood and fluid, screaming and crying. I gazed at him, transfixed, for what seemed like a moment or two. Finally I said, “I want to pick him up but I can’t.” My arms were supporting my body. Someone cranked up the back of the bed to support me and finally I held little Kevin against my body, skin to skin. He continued screaming. I tried to comfort him and to nurse him. One of the nurses was trying to suction out his nose. We had never bothered with suctioning during my home births. “R” cut the cord right away. I thought I had told her I believed in delayed cutting of the cord!
Soon the placenta was out. There was no excessive bleeding as seemingly everyone had feared. “R” told me that the baby’s cord had been wrapped around and under one of his shoulders and was getting somewhat compressed during labor, which is what explained the decelerations that had registered on the monitor. But he had an Apgar score of 9 and was screaming and healthy! He couldn’t have been very depressed! I wonder what kind of heart beat patterns my other babies would have had had I been monitored during my other labors.
Kevin had a long umbilical cord, and most interestingly, there was a true knot in the cord which “R” showed me. It was still loose, however. Whew! I’m glad we didn’t know about that until it was all over.
A large warming lamp was placed over me while I continued holding Kevin. Someone also placed a blanket over him. My perineum had torn because I pushed Kevin out so fast. I had routine episiotomies back when Eric and Jason were born, so I am weaker there. I have torn like that with all three of my subsequent births when I have tried to give birth without an episiotomy. “R” stitched me up. She also removed the internal monitor. She never did manage to get it into Kevin’s head. It had become hooked onto my cervix instead. I was thankful he hadn’t been traumatized in that manner. I wasn’t even aware of it inside me.
Kevin did not nurse immediately. (None of my babies have wanted to nurse immediately after being born. It has always seemed to take them an hour or so to get around to it.) A special examining table was right in the room beside my bed, and “R” placed Kevin on it to examine him. The heat lamp was placed over him. She did a routine newborn exam, Kevin weighed 7 lb. 12 oz.
 By now, about an hour had gone by since Kevin had been born. I drank some juice and was feeling stronger. Steve and each of the kids took turns holding Kevin, and so did Sherry and Susan. Then Kevin was back in my arms, still only wrapped in a blanket. Finally he nursed. He had been born just before midnight, at 11:48 p.m. By now it was past 1 a.m. and the kids were extremely tired. My family and friends were all getting ready to leave. The nurse put a diaper on Kevin and I dressed him in a nightgown and blanket that I had brought. I didn’t want him to wear the hospital’s clothes. (I was, however, surprised to see that they used a variety of colorful blankets and gowns and not the standard white ones that I had remembered from my previous hospital births.)
By now, about an hour had gone by since Kevin had been born. I drank some juice and was feeling stronger. Steve and each of the kids took turns holding Kevin, and so did Sherry and Susan. Then Kevin was back in my arms, still only wrapped in a blanket. Finally he nursed. He had been born just before midnight, at 11:48 p.m. By now it was past 1 a.m. and the kids were extremely tired. My family and friends were all getting ready to leave. The nurse put a diaper on Kevin and I dressed him in a nightgown and blanket that I had brought. I didn’t want him to wear the hospital’s clothes. (I was, however, surprised to see that they used a variety of colorful blankets and gowns and not the standard white ones that I had remembered from my previous hospital births.)
“That’s fine,” the nurse told me. “As long as you don’t get them mixed up with our laundry. If you do you’ll never find them again!”
The saddest part of being in the hospital was seeing my friends and family leave me. I ached to go home with my family as they went out the door. The kids needed their sleep and they would all be back to get me and Kevin in the morning. The hospital had a minimum requirement of four hours that the mother and baby had to stay following birth. (To me this seems extremely progressive! Only a few years ago leaving this early was totally unheard of! I recall getting a lot of “raised eyebrows” when I left the hospital two days after Eric’s birth back in 1972.) Had the baby been born during the day, leaving four hours later wouldn’t have been bad at all. But at this hour of the night I missed my family terribly and yearned to he with them. That was one of the nicest things about giving birth at home, to be able to settle down in my own home and environment immediately afterwards. Both Sherry and Susan had given birth at home themselves, and although they were quite impressed with the progressiveness of this hospital, they sympathized with my feelings. “I felt like we were deserting you.” Susan later told me.
Kevin was settled down to sleep in the little plastic bassinet next to my bed. I left to take a shower while the nurse cleaned up the room and changed the bed, I had insisted that the baby was not to go to the nursery as long as all was normal and they gave me no arguments about that. I took my shower and put on a fresh nightgown. The nurse was just finishing cleaning up the room when I got back. Kevin was still sleeping peacefully. By now it was about 2:30 a.m.
The nurse looked over the charts and noticed that “R” had not recorded his length. I picked him up so I could go to sleep with the baby in bed with me. I didn’t want him disturbed, but she carefully stretched him out just long enough to measure him. He remained asleep and oblivious to it all.
Then she looked at him worriedly and said, “Usually we like to run a tube down into the baby’s stomach right after birth to suction out his stomach contents.” She looked at me. “But since you’ve ordered no vitamin K or drops in his eyes, I suppose you don’t want us to do that either.”
I was aghast! “You suction out the baby’s stomach right after birth!!” I had never heard of any such thing. I looked at Kevin sleeping so peacefully and said, “I don’t think he needs that!”
After that we were left alone. Since I would be leaving in the morning and no one else was in labor, they left me there in the birth room for the night. The bed, which had been a perfectly satisfactory set up for giving birth, was terribly hard and uncomfortable for sleeping on. Also it was much too high to easily climb in and out of, both during labor and now with a sore perineum. I managed to sleep a little, but I.V.s pump a lot of fluids into one’s system and by 5 a.m. I awoke, desperately needing to go to the bathroom!! The baby was still peacefully sleeping, so I left him in bed. When I returned he had awoken a little and I got him to nurse again. By 6 a.m. the lab tech came by to take a sample of my blood. I might as well forget about getting any more sleep now.
I hadn’t been hungry right after giving birth but by this time I was ravenous. Breakfast trays would not be brought until 8 a.m. “M” came by to check me and the baby, We both excitedly talked about the birth. Since she lives in Bellingham too, we agreed that she would come over to my house in a couple of days to check on us again.
I watched TV and finally ate breakfast. That morning I heard another woman groaning in one of the other birth rooms. (This hospital doesn’t even have traditional labor rooms or delivery rooms. All of their vaginal births, prepared or not, take place in the birth rooms.) I heard the fetal heart monitor going and I was aware of the nurses scurrying around frantically. Over the intercom they were calling for medications and a surgery room was being set up “STAT!” A young girl had come in in her 7th month, in labor. She had had no prenatal care and now the baby was in trouble. They were doing an emergency Cesarean delivery and one of the nurses told me that they figured they would be able to save the mother but didn’t know if they could save the baby. Arrangements were being made to transport the baby to Seattle. I never did know the outcome of that birth.
At about 10 a.m. Steve and the kids finally showed up. It had taken them that long just to get up and get going. I had gotten everything into my suitcase and couldn’t wait to leave. There were a lot of papers to sign, birth certificate to fill out, etc. A nurse came in to fill out the forms. The she picked up Kevin and put black ink on his feet to take his footprints. Kevin screamed as she did this. Babies really don’t like to be messed with, even when it’s something that doesn’t hurt. We had signed several waivers. I insisted on no immediate PKU test, (which isn’t valid immediately after birth if the baby is breastfed) with the agreement that we would have it done at “R’s” birth center ten days later.
Finally we joyfully went home, to begin our life with our new baby. On Tuesday, 3 days after the birth, “M” came over to check on me and Kevin who was thriving and healthy. We talked some more about the birth and she said, “I knew, how badly you wanted a home birth I almost said to you, ‘Yes, I’ll go ahead and do your home birth for you if you want it.’ But I was afraid that if I did I’d get in trouble with “R” Now she tells me!! “M” does not regularly do home births, and I had no idea that she would even consider it!! So many of the decisions surrounding Kevin’s birth have centered around fear and politics!!
In retrospect, I am not unhappy about my birth experience. Following the extremely painful losses I have had, believe me, I was just delighted to have a live, healthy baby again. If I allow myself to feel any anger, I feel it towards to over conservativeness of the local home birth midwives I had approached. I don’t feel any anger towards the hospital which was unusually cooperative with making birth as homelike as possible. Most of the drawbacks cannot be helped. And like them, I too have been captive of the fear and over-cautiousness that perinatal loss brings which unavoidably affects our actions surrounding normal birth. There are some things I would have liked to have changed about Kevin’s birth, but then there are things about my two home births that I wish could have been different as well, such as the traumatic attempt at giving Lisa a Leboyer bath, or Ryan’s circumcision. (Kevin is intact, of course. No way would I ever again subject another son to the trauma of circumcision. So I’m certain Kevin is much better off than his home born, but circumcised older brother. )
My strongest concerns surrounding birth have centered around the baby’s needs and feelings. What gets done to me, such as having an I.V. in my arm, are less crucial in my opinion. Although I had to be knowledgeable and assertive about some things, such as insisting on no eye drops, vitamin K, or separation from the baby, I feel that hardly any compromises were made as to how Kevin was treated. However accommodating, there were some definite disadvantages about hospital birth from my perspective, such as the ride there and back and being without my family immediately after birth. But I do not believe that those things which made a difference to me, made any difference to the baby. A baby’s awareness is different from ours. A newborn baby is aware of being held securely and of being kept close to his mother and those that love him. He is unhappy if he is not fed when he is hungry, or put in traumatic, compromising, or uncomfortable situations. However, as long as these needs are met, I do not believe that a baby has any perspective of where they are, the way an older child or an adult does. Surely a traditional hospital setting, where the baby is kept away from his mother in the nursery and subjected to rigid feeding schedules and traumatic procedures does make a profound difference to the baby. But in a setting like I was able to have for Kevin, I doubt that location per se makes any difference to the baby.
The question arises as to what I would do if I should ever have another baby.* This has got to be purely academic as five children are a tremendous amount of responsibility and expense. Also, I am not getting any younger. But if it should ever happen, I would still be interested in having another home birth. Kevin’s birth could have been at home. There were no complications. I do have regrets that I was unable to convince others that all would go okay. I also sometimes wish I had been able to either do it on my own or with a less qualified midwife. But if I were ever to have another baby, it would be my sixth and I would be in my forties. The ultra conservative home birth midwives in this area automatically turn anyone down on either one of those two accounts. I would also be willing to give birth again in that hospital, or any similarly homelike setting. However, as much as I liked and respected “R”, I would seek a birth attendant who was less dependent on the fetal heart monitor. I feel that I made a mistake in assuming that a midwife, simply by virtue of being a midwife, would automatically be as non-interventive as I would have liked.
In 1977 when I had Ryan at home, options within the hospital, such as including older children and friends for hospital or birth center birth, wearing one’s own nightgowns, giving birth in a bed, and most importantly having immediate, unhampered bonding with the baby was not available beyond our wildest dreams! Today that gap has narrowed dramatically. Perhaps if this type of setting had been available for birth back then, I might never have taken an interest in home birth. On the other hand, I could never have gone back to a traditional “labor room – delivery room, flat on your back, legs in stirrups, baby whisked off to the nursery” type of birth. I’m sure that had this type of extremely progressive type of birthing option not been available within the hospital, I would have gone ahead and given birth at home on my own or with an untrained midwife, despite my fears.
…………
*Update: There is a joyful “sequel” to this story. Four years later, in 1989, I gave birth to our sixth child, another daughter – Melissa, at home in our bathtub. We had moved to Anchorage, Alaska the previous year. When I became pregnant again I found that the midwives in this community were not nearly as fearful or conservative as the ones I had dealt with in Washington state, despite my age (42 at that time) and prior history. The story of her birth is recounted in “Melissa’s Birth” which also appears on this website. – R.R. Click here for article.

Kevin with big sister, Lisa, at about 4 months old.

Kevin, fat and sassy at about 7 months.

Kevin – “all boy” – at about 9 months.

Kevin at age 4, now “different” because he wears glasses. (Okay, by now Mom and Dad need reading glasses!) Should the rest of the kids get glasses so we can all “match?”